Hip
Hip Anatomy
The hip joint is the largest weight-bearing joint in the human body. It is also referred to as a ball and socket joint and is surrounded by ligaments, muscles, and tendons. The thigh bone or femur and the pelvis join to form the hip joint.
Injury or disease of the hip can adversely affect the joint's range of motion and ability to bear weight.
The hip joint is made up of the following:
- Bones and cartilage
- Ligaments of the joint capsule
- Muscles and tendons
- Nerves and blood vessels that supply the bones and muscles of the hip
Bones & Cartilage
The hip joint is the junction where the hip joins the leg to the trunk of the body. It is comprised of two bones: the thigh bone or femur and the pelvis. The ball of the hip joint is made by the femoral head while the socket is formed by the acetabulum. The Acetabulum is a hemispherical socket formed on the outer edge of the pelvis by the union of three bones: ilium, ischium and pubis. The stability of the hip is provided by the joint capsule, labrum, and muscles that surround the joint.
The head of the femur rotates and glides within the acetabulum. A fibrocartilaginous bumper called the labrum is attached to the rim of th acetabulum and further increases the depth of the socket.
The femur is the longest bone in the body. The upper part of the femur consists of the femoral head, neck, and greater and lesser trochanters. The head of the femur joins the pelvis (acetabulum) to form the hip joint. Next to the femoral neck, there are two protrusions known as greater and lesser trochanters which serve as sites of muscle attachment.
Articular cartilage is the thin, smooth, flexible, and slippery surface lubricated by synovial fluid that covers the bones within our joints. It enables smooth movements of the joints and reduces friction when healthy.
Ligaments
Ligaments are strong fibrous structures that connect bones to other bones. The hip joint is encircled with ligaments to provide stability to the hip by forming a dense and fibrous structure around the joint capsule. The ligaments adjoining the hip joint include:
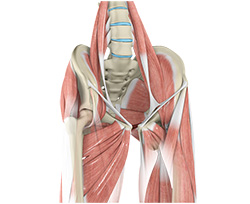
Muscles & Tendons
- IT Band - A long tendon called the iliotibial band runs along the outside of femur from the hip to the knee. It originates from the gluteus maximus and the tensor fascia latae.
- Gluteals - These are the muscles that form the buttocks. There are three muscles (gluteus minimus, gluteus medius, and gluteus maximus) that attach to the back of the pelvis and insert into the greater trochanter of the femur.
- Adductors - These muscles are on the inner aspect of the thigh and function to pulll the leg back towards the midline.
- Iliopsoas - This muscle is in front of the hip joint and provides flexion. It is a deep muscle that originates from the lower back and pelvis, and inserts on the lesser trochanter.
- Rectus femoris - This is the largest band of muscles located in front of the thigh called the quadriceip. The rectus femoris is another important hip flexor.
- Hamstrings - These begin at the bottom of the pelvis and run down the back of the thigh. Because they cross the back of the hip joint, they help in extension of the hip by pulling it backwards.
Nerves & Arteries
Nerves of the hip transfer signals from the brain to the muscles to aid in hip movement. They also carry the sensory signals such as touch, pain, and temperature back to the brain.
The main nerves in the hip region include the femoral nerve in the front of the femur and the sciatic nerve at the back. The hip is also supplied by a smaller nerve known as the obturator nerve.
In addition to these nerves, there are blood vessels that supply blood to the lower limbs. The femoral artery, one of the largest arteries in the body, arises deep in the pelvis and can be felt in front of the upper thigh.
Hip Movements
All the anatomical parts of the hip work together to enable normal function. Hip movements include flexion, extension, abduction, adduction, and internal/external rotation.
Understanding Hip Pain
Osteoarthritis :: Rheumatoid Arthritis :: Post-Traumatic Arthritis
Osteoarthritis
The thigh bone (femur) joins the pelvis (acetabulum) to form a ball and socket joint called the hip. Ligaments, which are strong bands of tissue that connect bone to bone, are the main providers of joint stability. Tendons, which are bands of tissue that connect muscle to bone, are secondary stabilizers of the joint. Muscles, ligaments, and tendons work together to complete the kinetic chain.
A smooth substance called articular cartilage covers the surface of the bones where they come into contact within the joint. This articular cartilage acts as a cushion between the bones. The remainder of the inside of the hip joint is covered by a thin, smooth tissue liner called synovium. The synovium makes a small amount of fluid that acts as a lubricant so that the joint glides smoothly.
One of the most common causes of hip pain and loss of mobility is the wearing away of the joint’s cartilage. When this happens, the bones rub against each other, causing significant pain and swelling. The most common cause is a condition known as osteoarthritis. Trauma or direct injury to the knee can also cause osteoarthritis. Without cartilage there is no shock absorption between the bones in the joint, which allows inflammation to build and contribute to pain.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s natural immune response attacks the lining of the joints (called the synovium), causing chronic inflammation and pain. The inflammation may eventually damage the joint’s cartilage and bone, weaken the soft tissue around the joint (cartilage, ligaments and tendons) and prevent the joint from working properly.
Left untreated, RA can greatly reduce your quality of life. You may have already decreased your activity level to avoid the pain caused by a joint affected by RA. It’s not uncommon for the joint damage caused by RA to lead to a loss of movement, an inability to work, and even the need for surgery to repair the damage.
What are the Symptoms of RA?
RA is a chronic, persistent disease that can take a variable course over an affected person’s lifetime. It may progress slowly, sometimes produce “flare ups”, and then at times go into “remission” during which the symptoms may greatly diminish or disappear. There are 3 stages of RA identified by specific symptoms. In the first stage, RA causes pain, warmth, redness and swelling in affected joints. In the second stage, it causes thickening of the synovium. In the third stage, permanent joint damage begins to occur as bone and cartilage are attacked by the enzymes released by the inflamed cells in the once-healthy synovial fluid.
In addition to joint pain, swelling and stiffness, the symptoms of RA commonly include fatigue, weakness, flu-like symptoms accompanied by a low-grade fever, loss of appetite, depression, chronic dry eye or dry mouth and, in people with more advanced RA, bumps (called rheumatoid nodules) under the skin.
How is RA Treated?
Your primary doctor will refer you to a rheumatologist, a doctor who specializes in inflammatory diseases like RA. Your rheumatologist may recommend different treatment options depending on the severity of your RA and its impact on your joint(s) and your body as a whole. And while there is no cure, RA can be controlled through the use of new drugs, exercise, and self-management techniques.
If your RA is so severe that conservative treatment options are no longer managing your symptoms to meet your activity goals, joint replacement may be an option. Some treatment options, such as partial hip replacement, are not indicated for patients with RA because the underlying disorder will inevitably affect the other native parts of the hip. Dr. Fischer will work with you and your other physicians to develop an individual treatment plan
Post-Traumatic Arthritis
Post-traumatic arthritis is caused by the wearing out of a joint that has had any kind of physical injury. The injury could be from sports, a vehicle accident, a fall, a military injury, or any other source of physical trauma. Such injuries can damage the cartilage and/or the bone, changing the mechanics of the joint and making it wear out more quickly. The wearing-out process is accelerated by continued injury and excess body weight.
What Are The Symptoms of Post-Traumatic Arthritis?
The symptoms of post-traumatic arthritis include joint pain, swelling, fluid accumulation in the joint, and decreased tolerance for walking, sports, stairs and other activities which stress the joint.
How is Post-Traumatic Arthritis Treated?
Post-traumatic arthritis is treated similarly to osteoarthritis. Treatment starts with weight loss, low impact exercise and strengthening of the muscles surrounding the joint, non-steroidal anti-inflammatory medicines (NSAIDs such as Advil, Aleve, Celebrex or one of many others) are often recommended if you can take them. Arthritic joints can also be injected with cortisone or substances called Hylamers which act like artificial joint fluid. All of these measures are aimed at making the joint more comfortable and functional. They do not cure the arthritis.When the arthritis progresses to the point that these measures are not effective in treating pain and maintaining function, then surgical treatment will be discussed.
Surgical treatment may include debriding ("cleaning out"), reconstructing or replacing the worn out joint surfaces. Post-traumatic arthritis progresses as time goes on, the joint surface wearing out further with more use over the years. Fortunately, when the nonsurgical treatments are no longer effective, surgical treatment can offer lasting relief. Deformity through or around the joint may necessitate the use of computer assisted navigation to restore the joints normal alignment.
Treating Hip Pain
Dr. Fischer may recommend different treatment options depending on the severity of your arthritis and your specific activity goals.
Treatment starts with weight loss, low impact exercise and strengthening of the muscles surrounding the joint, non-steroidal anti-inflammatory medicines (NSAIDs such as Advil, Aleve, Celebrex or one of many others) are often recommended if you can take them. Arthritic joints can also be injected with cortisone or substances called Hylamers which act like artificial joint fluid. All of these measures are aimed at making the joint more comfortable and functional. They do not cure the arthritis. When the arthritis progresses to the point that these measures are not effective in treating pain and maintaining function, then surgical treatment will be discussed.
Dr. Fischer will determine the proper surgical treatment based on the severity of your arthritis and its location. Today, a full range of surgical solutions exist that enable Dr. Fischer to tailor the treatment to your particular needs and anatomy.
Surgical Treatment Options
Conditions
Hip Injuries & Tears

Snapping Hip
The hip is an important joint that helps us walk, run and jump. The ball-and-socket joint in the hip is formed between the round end of the femur (thighbone) and the cup-shaped socket of the acetabulum (part of the hip bone). Joint stability in the hip region is achieved through the labrum (a strong fibrous cartilage), which covers the acetabulum and seals it, and ligaments (tissue connecting bone to bone) and tendons (tissue connecting muscle to bone) that encase the hip and control the hip movements.

Hip Pain
Hip pain, one of the common symptoms patients complain of, may not always be felt precisely over the hip joint. Pain may be felt in and around the hip joint and the cause for pain is multifactorial. The exact position of your hip pain suggests the probable cause or underlying condition causing pain. Pain felt inside the hip joint or your groin area is more likely to be because of the problems within the hip joint.
Muscle Strains
A tear in the muscle fibers caused by either a fall or direct blow to the muscle, overstretching and overuse injury is called a strain. Muscle strains often occur in the hip region whenever a muscle contracts suddenly from its stretched position. It can be mild, moderate or severe and depends on the level of injury. The chances of having a hip muscle strain becomes high if you have had a previous injury in the area or if there is no warm-up before exercising.

Femoroacetabular Impingement
Femoroacetabular impingement (FAI) is a condition where there is too much friction in the hip joint from bony irregularities causing pain and decreased range of hip motion. The femoral head and acetabulum rub against each other creating damage and pain to the hip joint. The damage can occur to the articular cartilage (the smooth white surface of the ball or socket) or the labral tissue (the lining of the edge of the socket) during normal movement of the hip.
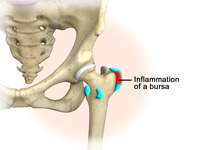
Hip Bursitis
Hip bursitis is a painful condition caused by inflammation of a bursa in the hip. Bursae are fluid filled sacs present in joints between bone and soft tissue to reduce friction and provide cushioning during movement.
The bony prominence of the hip is called greater trochanter and is present on the outer side of the upper thigh bone or femur. The bursa overlying it is called trochanteric bursa. Another bursa is located towards the groin region and is called iliopsoas bursa. Bursitis of the trochanteric bursa is more common than that of iliopsoas bursa.
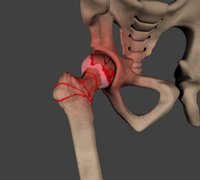
Avascular Necrosis
Avascular necrosis, also called osteonecrosis is a condition in which bone death occurs because of inadequate blood supply to it. Lack of blood flow may occur when there is a fracture in the bone or a joint dislocation that may damage nearby blood vessels. Chronic use of high doses of steroid medications and heavy alcohol consumption are the two main risk factors of avascular necrosis. Initially, small breaks appear in the bone that may eventually collapse.

Hip Fracture
The hip joint is a “ball and socket” joint. The “ball” is the head of the femur, or thigh bone, and the “socket” is the cup shaped acetabulum. The joint surface is covered by a smooth articular surface that allows pain free movement in the joint.

Hip Dislocation
The hip joint is a ball and socket joint. The “ball” is the head of the femur, or thigh bone, and the “socket” is the cup shaped acetabulum. The joint is surrounded by muscles, ligaments, and tendons that support and hold the bones of the joint in place. Hip dislocation occurs when the head of the femur moves out of the socket.
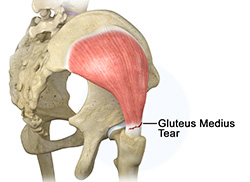
Gluteus Medius Tear
A gluteus medius tear is a condition characterized by severe strain on the gluteus medius muscle that results in partial or complete rupture of the muscle.
The gluteus medius is one of the major muscles of the hip and is essential for movement of the lower body and keeping the pelvis level during ambulation.

Hip Labral Tear
A hip labral tear is an injury to the labrum, the cartilage that surrounds the outside rim of your hip joint socket. The hip joint is a ball and socket joint in which the head of the femur is the ball and the pelvic acetabulum forms the socket. The labrum helps to deepen the socket and provide stability to the joint. It also acts as a cushion and enables smooth movements of the joint.
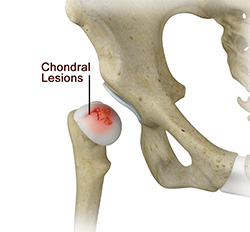
Chondral Lesions or Injuries
The hip joint is one of the largest weight-bearing joints in the body, formed by the thigh bone or femur and the acetabulum of the pelvis. It is a ball and socket joint with the head of the femur as the ball and the pelvic acetabulum forming the socket. The joint surface is covered by a smooth articular cartilage which acts as a cushion and enables smooth movements of the joint. A chondral injury refers to an injury of the articular cartilage, covering the joint.

Hip Instability
The hip plays an important role in supporting the upper body weight while standing, walking and running, and hip stability is crucial for these functions. The femur (thigh bone) and acetabulum (hip bone) join to form the hip joint, while the labrum (tissue rim that seals the hip joint) and the ligaments lining the hip capsule maintain the stability of the hip.
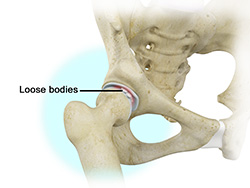
Loose Bodies
Loose bodies are small loose fragments of cartilage or a bone that float around the joint. The loose bodies can cause pain, swelling, locking and catching of the joint. Loose bodies occur if there is bleeding within the joint, death of tissues lining the joints associated with tuberculosis, osteoarthritis, and rheumatoid arthritis. Other causes include fractures, trauma, bone and cartilage inflammation, and benign tumors of the synovial membrane.

Hip Groin Disorders
Hip and groin disorders are more common in athletes, caused by rapid acceleration and deceleration motion.
The rehabilitation time for hip and groin injuries are longer than most other injuries, therefore early and accurate diagnosis is essential. The management of hip and groin injuries is complex due to the presence of multiple anatomic structures in that region.

Subtrochanteric Hip Fracture
A hip fracture is a break that occurs near the hip in the upper part of the femur or thigh bone. The thigh bone has two bony processes on the upper part - the greater and lesser trochanters. The lesser trochanter projects from the base of the femoral neck on the back of the thigh bone. Hip fractures can occur either due to a break in the femoral neck, in the area between the greater and lesser trochanter or below the lesser trochanter.

Hip Abductor Tears
Hip abductors are a major group of muscles found in the buttocks. It includes the gluteus maximus, gluteus medius, gluteus minimus, and tensor fascia lata muscles.
The Gluteus medius arises at the top of the pelvic bone and runs to attach on the outer side of the thighbone or femur. The muscle controls side-to-side movement of the hip and stabilizes hip movement.

Hip Synovitis
Hip synovitis, also called transient hip synovitis or toxic synovitis is a condition in which there is inflammation of the synovial tissues surrounding the hip joint causing hip pain. It is the most common reason for sudden hip pain occurring in young children between the age of 2 and 9. It affects boys more commonly than girls and most of the times, the hip joint on only one side is affected.

Irritable Hip
Irritable hip, also known as acute transient synovitis, is a common disorder of childhood characterized by onset of hip pain and limping. The term transient means that it does not usually last long. It usually occurs before puberty and affects only one hip. Boys aged between 4 to 10 years are most often affected 2 to 4 times more than girls.

Hip Tendonitis
Tendons are strong connective tissue structures that connect muscle to bone. Hip tendonitis is a condition associated with degeneration of the hip tendons. This condition is mainly caused due to strain on the tendons which may be due to overuse, or biomechanical problems.

Hip Pointers
The hip joint consists of 2 bones, the hip bone and the leg bone. An injury or bruise to one of these bones or the surrounding muscles or tissues is termed a hip pointer. This type of injury is mainly caused due to a sudden blow or hit on the hip which can occur from sports activities such as football, rugby, volleyball, basketball, cycling or skating.

Developmental Dysplasia
Developmental dysplasia of the hip (DDH) or Hip dysplasia is a condition which is seen in infants and young children because of developmental problems in the hip joint. The femur (thigh bone) partially or completely slips out of the hip socket causing dislocation at the hip joint. It is most common in first born baby with family history of the disorder.

Legg-Calve-Perthes-Disease
Legg-Calve-Perthes Disease (LCPD) or Perthes disease is a disorder of the hip that affects children, usually between the ages of 4 and 10. It usually involves one hip, although it can occur on both sides in some children. It occurs more commonly in boys than girls.
Hip Arthritis

Osteoarthritis of the Hip
Osteoarthritis, also called degenerative joint disease is the most common form of arthritis. It occurs most often in older people. This disease affects the tissue covering the ends of bones in a joint (cartilage). In a person with osteoarthritis, the cartilage becomes damaged and worn out causing pain, swelling, stiffness and restricted movement in the affected joint.
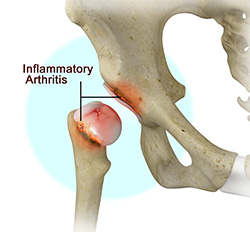
Inflammatory Arthritis of the Hip
Inflammation of the joints is referred to as arthritis. The inflammation arises when the smooth covering (cartilage) at the end surfaces of the bones wears away. In some cases, the inflammation is caused when the lining of the joint becomes inflamed as part of an underlying systemic disease. These conditions are referred to as inflammatory arthritis.

Transient Osteoporosis of the Hip
Transient osteoporosis of the hip is a rare condition that causes bone loss temporarily in the upper part of the thighbone (femur). It is mostly found in young or middle aged men between the ages of 30 and 60, and women in their later stages of pregnancy or early postpartum period (following childbirth). It is characterized by abrupt onset of pain that increases with activity.
Procedures
Non-Surgical Treatments
Hip Injections
Hip joint injections involve injecting medicine directly into the hip joint to diagnose the source of pain or treat pain due to conditions such as arthritis, injury or mechanical stress of the hip joint. Hip pain may be experienced in the hip, buttock, leg or low back. The injection contains a combination of a numbing medicine and cortisone (an anti-inflammatory agent).
Physiotherapy
Physiotherapy or physical therapy is an exercise program that helps you to improve movement, relieve pain, encourage blood flow for faster healing, and restore your physical function and fitness level. The main aim of physical therapy is to make your daily activities, such as walking, getting in and out of bed, or climbing stairs, easier.
Platelet Rich Plasma Therapy
Our blood consists of a liquid component known as plasma. It also consists of three main solid components which include the red blood cells (RBCs), white blood cells (WBCs), and platelets. Platelets play an important role in forming blood clots.
Surgical Treatment
Hip Fracture Repair
Surgical correction of a hip fracture is known as hip fracture surgery.
Hip fractures involve a break that occurs near the hip in the upper part of the femur or thigh bone. The thigh bone has two bony processes on the upper part - the greater and lesser trochanters. The lesser trochanter projects from the base of the femoral neck on the back of the thigh bone. Hip fractures can occur either due to a break in the femoral neck, in the area between the greater and lesser trochanter or below the lesser trochanter.
Hip Replacements
- Total Hip Replacement
- Direct Superior Approach
- Direct Superior Hip Replacement
- Revision Hip Replacement
- Outpatient Hip Replacement
- Partial Hip Replacement
- Fracture Repair around a Hip Replacement
Others
Hip FAQs
How long will I stay in the hospital?
You will likely stay in the hospital for 1 night depending on your preoperative conditioning and your pace of mobilization. This is highly dependent upon your condition before surgery, your age, and medical problems which can slow your rehabilitation. Patients who are otherwise healthy are eligible for a rapid recovery and discharge to home the day of surgery.
When can I walk after surgery?
The goal is to get out of bed with physical therapy the day of surgery. Most people are walking with the assistance of a walker on the day after surgery, and using a cane or nothing at all by 2-3 weeks.
How often will I see my surgeon after surgery?
Dr. Fischer is in charge of your care throughout your hospital stay. You can expect to see Dr. Fischer every day while you’re in the hospital recovering. Dr. Fischer will also want to see you for follow-up appointments in his clinic after you are discharged. Follow-up appointments are scheduled 2 weeks after surgery. Further appointments will be made and the timing is based on each individual's needs.
Will I need physical therapy after my hip replacement?
Maybe. Most of the time a home exercise program is all that is required after a primary hip replacement. Formal physical therapy may be a necessary part of your recovery if you have a particular goal in mind. Physical therapy may be performed in the outpatient setting, in your home, or in a rehabilitation facility depending on your individual needs.
Is hip replacement very painful?
Pain management following total hip replacement has come a long way with increased use of preoperative medication, spinal blocks, and multimodal pain control. Total hip replacement is generally considered to be less painful than total knee replacement. Early range of motion and rapid rehabilitation protocols are also designed to reduce early stiffness and pain, making the procedure in general much less painful than in years past. You may have relatively mild pain following the procedure, or you may have a more difficult time than others. Everyone is unique and handles and perceives pain differently.
Will I need general anesthesia?
While general anesthesia is a safe option, both hip and knee replacements can be performed under regional anesthesia. Choices for regional anesthesia include spinal anesthesia, epidural anesthesia, or one of a variety of peripheral nerve blocks. Many surgeons and anesthesiologists prefer regional anesthesia because data shows it can reduce complications and improve your recovery experience with less pain, less nausea, less narcotic medicine required, etc.
When can I take a shower or bath at home?
Showering (not submerging the wound) is typically allowed immediately after surgery with the water resistant dressing in place. When you return home, you may need special equipment, like a bath mat, hand-held showerhead or shower seat to help you shower comfortably and safely. Taking a bath (submerging the wound) is only allowed after the wound has completely healed over and all scabs have disappeared.
When will I be able to drive again?
You should not drive a car or other motor vehicle until Dr. Fischer has approved. You must be off pain medications before you will be cleared to drive again. In most cases, patients are able to resume driving 2 weeks after surgery.
How should I sleep at night to keep my hip comfortable and safe?
You may sleep however you feel most comfortable. Placing a pillow between your legs may improve your comfort until the hip heals.
How long does it take to recover?
It can take up to 3 months for you to return to most activities, and likely 6 months to one year to fully recover to maximal strength and endurance following a hip replacement. This depends on your condition before surgery, additional medical problems, and your expectations.
How do I know if my incision is infected?
After surgery you will notice some redness, bruising, swelling and warmth around your incision. This is normal. If you experience spreading redness, increasing swelling, or persistent drainage from you incision, you may have an infection. A persistent fever greater than 101°F may also indicate infection. A Surgeon is on call 24/7 to address any questions or concerns you may have.
Why must I take antibiotics for dental work or other surgical procedures?
Taking antibiotics is a precaution to help ensure that your new artificial joint does not become infected. Additional surgeries or dental work increases the chance of infection. No matter where the infection starts, if it spreads to your new hip, the results can be serious. When artificial joints become infected, they must be removed surgically and then replaced months later. Please let your other medical providers know that you have had joint replacement.
What is the lifespan of a hip replacement?
All implants have a life expectancy that depends on several factors including the patient’s weight, activity level, quality of bone stock and compliance with the surgeon’s orders. Proper implant alignment and state of the art materials also contribute to a replaced joint's longevity. With modern bearing materials, a 20-30 year implant life is probable.
Do you use metal on metal implants?
Dr. Fischer does not use Metal on Metal implants for hip replacements. The hip implants Dr. Fischer uses are state of the art ceramic or cobalt chrome (metal) on highly cross linked polyethylene (high density plastic).
What if I have a nickel allergy?
Dr. Fischer routinely uses a nickel free hip replacement that avoids the potential complications to patients who are allergic or sensitive to nickel.
